LGBTQ+
Our
Vision
ABOUT US
The UCLA Center for LGBTQ+ Advocacy, Research & Health, or C-LARAH (LARAH is derived from the Latin word “hilaris,” meaning cheerful) is dedicated to improving the health and well-being of sexual and gender minorities. We are committed to sharing our expertise in public health, including epidemiological methods, developing and testing bio-behavioral interventions, education and research training, program design and analysis, health policy initiatives and implementation science.
We work directly with members of the LGBTQ+ community and are able to draw upon expansive local and national relationships with state and local public health departments, academic researchers, healthcare providers, community-based organizations, consumer groups, advocacy foundations, and funding agencies.
Our familiarity and experience working with the LGBTQ+ community and allied organizations well-equips us to inform policymakers of the most effectual ways to reach members of this historically marginalized population and how to serve them holistically through all social determinants of health and justice.
Mission Statement
To maintain an interdisciplinary, research-driven, evidence-based platform used to carry out public policy initiatives that improve the health and social well-being of sexual and gender minorities. We engage our local and national community, as well as global partners, through cross-culturally informed scholarship, advanced academic training, and civic advocacy. We are deeply invested in intercultural competence and the importance of intersectionality of identities and lived experience; we are committed to conducting research to advance LGBTQ+ racial/ethnic health disparities.
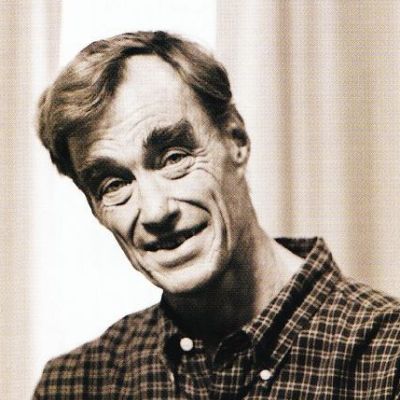
DR. MATTHEW J. MIMIAGA
DIRECTOR’S MESSAGE
“Sexual and gender minorities experience significant health disparities as a result of myriad overlapping social-ecological, cultural, and political factors. Research findings by our team and others show that LGBTQ+ populations have a higher prevalence and incidence of life-threatening physical conditions, mental health problems, substance use, and chronic and infectious disease risk. Despite recent advances to civil rights protections, LGBTQ+ individuals continue to experience elevated rates of stigma, discrimination and violence. They are disproportionately represented among homeless people—often a result of estrangement from their families—and face significant barriers to accessing health care, prevention and treatment services. Now is the time for academic institutions to bolster the unwavering efforts at progress made by the LGBTQ+ movement. We must bridge health, research, and training measures to curtail socioeconomic inequities and close the health disparity gap. We have spent the past four decades advocating for LGBTQ+ rights—indeed, for their basic humanity—and we must continue to demand accountability in shaping and enforcing policies that best serve our community. It is extremely rewarding to be involved in work that improves the lives of historically marginalized members of society. I’m excited about the impact C-LARAH has had and will continue to have in training future generations of scientists interested in conducting LGBTQ+ public health and clinical research and ensuring that all sexual and gender minorities, and particularly those of us who are trans, racial/ethnic minorities and living with HIV, belong everywhere and can live openly and authentically, and be healthy.”
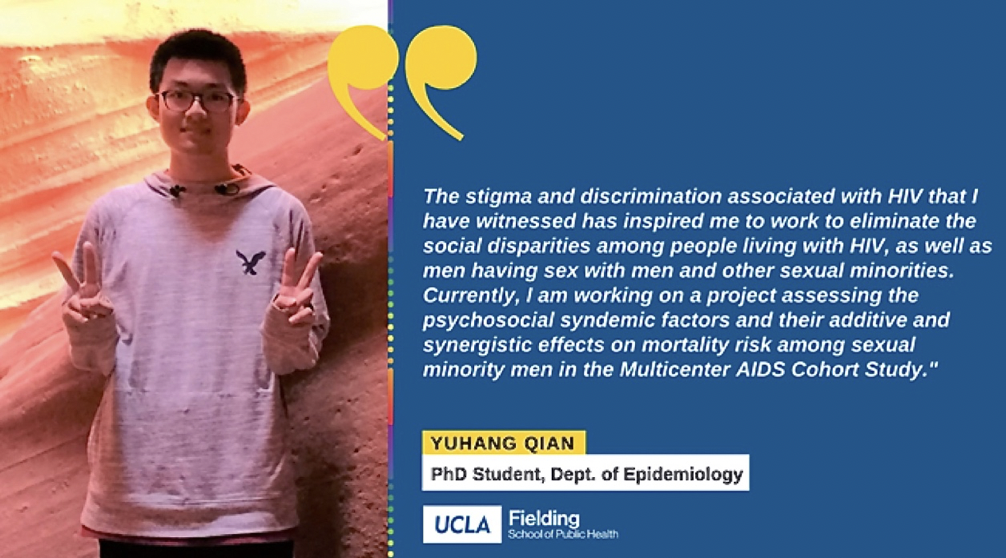
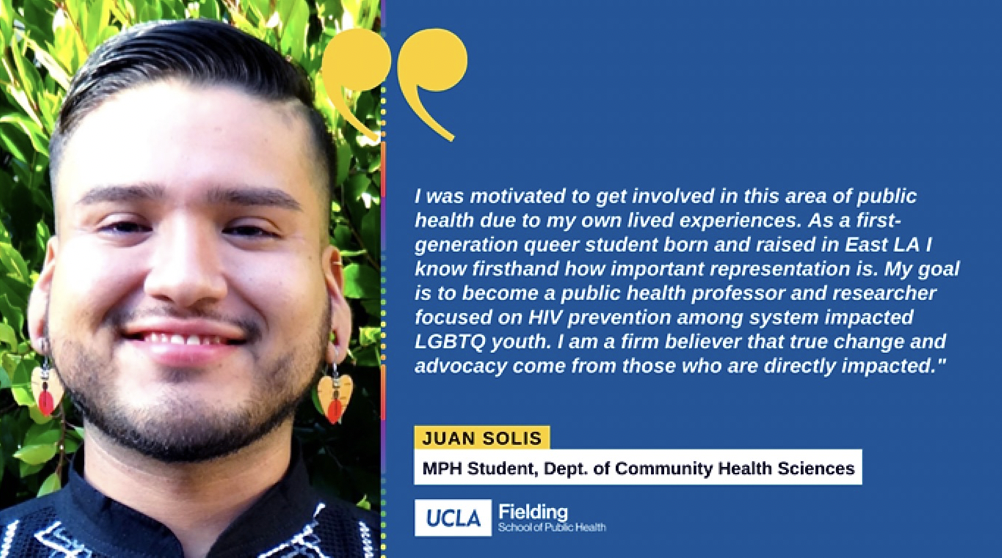
Research Training: Equity, Diversity & Inclusion
C-LARAH is committed to a collaborative and inclusive environment where students, post-doctoral fellows, and other mentees from diverse backgrounds are trained to thrive as leaders in LGBTQ+ public health, epidemiological methods, and behavioral science, and where students, postdocs, staff and faculty are valued regardless of race, ethnicity, religion, socio-economic position, first-generation college student, immigration status, gender identity, sexual identity, or disability.
C-LARAH is devoted to recruiting and training a community of diverse scholars from underrepresented minority groups and fostering a welcoming, inclusive and intellectually-enriching environment where all students, postdocs, staff and faculty feel supported and can achieve their full potential. Furthermore, we are dedicated to prioritizing our reach and understanding of diverse populations and communities in our research, scholarship and training programs, and advancing diversity, equity and inclusion in the field of LGBTQ+ public health.
Promoting research excellence and addressing diversity in our work setting is integral to our initiatives as a Center. It broadens and deepens the training experience and scholarly environment for students, postdocs and faculty alike. Our primary commitment to our students and postdocs is to provide an all-encompassing research training experience that is based on the principles of equity and inclusion of all individuals; within the Center environment, differences are acknowledged as contributions and individuals are respected for their beliefs and cultural practices.
Happy Pride 2024!
As we raise the rainbow flag high and wear our colors with pride, let us remember the profound significance of this momentous celebration. Pride is not merely a parade or a festival; it is a testament to the resilience, bravery, and unwavering spirit of the LGBTQ+ community. It stands as a symbol of defiance against discrimination, a beacon of hope for those who are still fighting for acceptance, and a reminder that love knows no bounds.
In the face of adversity and prejudice, Pride empowers us to stand tall and embrace our true selves unapologetically. It is a declaration of self-worth, a celebration of diversity, and a call to action for equality and justice. Through our visibility and unity, we amplify voices that have been silenced and pave the way for a brighter, more inclusive future for all.
In celebrating Pride, we acknowledge the progress made, yet remain steadfast in our commitment to advancing social justice and inclusivity for marginalized communities. Let us use this moment to reflect on the historical significance of Pride, honor the pioneers who have paved the way for progress, and recommit ourselves to the pursuit of a more equitable and affirming society for all. Happy Pride 2024 to each and every member of the LGBTQ+ community and its allies!
West Hollywood Pride and Los Angeles Pride in the Park, 2024
UCLA Epidemiology/C-LARAH PhD Students and Postdoctoral Fellows at WeHo Pride, 2024! Volunteering their time and expertise to work on HIV prevention initiatives for the LGBTQ+ community and exemplifying the best of dedication, compassion, and knowledge coming together for a noble cause. Their commitment to advancing LGBTQ+ public health and HIV and STI prevention is truly inspiring. Through their tireless efforts, they continuously demonstrate a profound sense of social responsibility and a deep-seated desire to create a more equitable and healthier world.
AND
C-LARAH Crew at LA Pride in the Park, 2024! Organized by Christopher Street West, the LA-based nonprofit that is responsible for achieving the world’s first permitted parade advocating for gay rights on June 28, 1970 to commemorate the Stonewall Rebellion on Christopher Street in New York City the year prior. Now, more than 50 years later, they have built a rich history as an active voice for the LGBTQ+ community across the Greater Los Angeles area, and we were excited to be a part of it!
The
Team
- CENTER FACULTY, STAFF & STUDENTS
- UCLA Faculty Affiliates
- Main Collaborators
- C-LARAH / UCLA Alumni .people-grid
Our Projects

PrEPare for Work
Optimizing PrEP Uptake & Adherence Among MSW Using a 2-Stage Randomization Design, 2016-2020
MPI: Mimiaga, Biello & Chan
National Institute of Mental Health (R34MH110369-01 + diversity supplement)
we designed the “PrEPare for Work” package that includes two components: 1) peer-led strengths-based case management (SBCM) for PrEP uptake, and 2) a counseling and problem-solving PrEP adherence intervention that addresses individualized barriers to optimal use. We conducted a pilot RCT of “PrEPare for Work” using a two-stage randomization design. Stage 1: 106 MSW were equally randomized to receive either the peer-led SBCM or standard of care (i.e., passive referrals only) for engagement with our existing PrEP clinic. Stage 2: Those from stage 1 who initiated PrEP (n~44), regardless of stage 1 randomization condition, were equally randomized to either the “PrEPare for Work” adherence intervention or standard of care comparison condition.
Findings provide evidence of feasibility and acceptability, and demonstrate initial efficacy for PrEP uptake and adherence.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper: Under Review
Secondary Outcome Paper 1
Secondary Outcome Paper 2

Project IMPACT
Name of Grant
Integrated behavioral activation and HIV risk reduction counseling for MSM with stimulant abuse
Funding Source
National Institute on Drug Abuse (R01DA042805-01A1)
Pls
Mimiaga and Safren
Background
Problematic stimulant (i.e., crystal methamphetamine [meth], cocaine, crack) use is a prevalent and treatment refractory problem in some men who have sex with men (MSM), and highly predictive of both condomless sex and HIV infection. This application builds off of our successful formative and pilot work and is designed to assess the efficacy, in a two-arm randomized controlled trial (RCT), of Project IMPACT—a behavioral intervention to reduce high-risk sex in MSM with stimulant use disorder who are at risk for HIV acquisition. The intervention incorporates risk reduction counseling with behavioral activation (BA) to help participants re-engage in enjoyable and meaningful life activities not involving drugs. Behavioral activation is an evidence-based, easy to administer, cognitive behavioral approach to treat depression and other problems that focuses on helping individuals reengage in activities that generate feelings of enjoyment (i.e., mastery and pleasure). We chose this strategy for MSM with stimulant use disorder because our formative work revealed that MSM who abuse stimulants report becoming unable to enjoy activities that they previously enjoyed as a result of ongoing stimulant use. This lack of enjoyment (i.e., anhedonia, one of the core symptoms of depression) in activities that do not involve stimulant use or sex contributes to the continued use of stimulants and potentially condomless sex (not protected by PrEP). We developed and openly field-tested this intervention in a NIDA-funded nonrandomized pilot (R03 DA023393), and, subsequently, conducted a NIDA-funded pilot RCT (R34 DA031028) of this intervention compared to a standard of care condition (SOC) and found it to be feasible, acceptable, and successful at reducing both condomless anal sex and stimulant use. The proposed efficacy trial is the next logical step in this program of research.
Conceptual Model
The conceptual model focuses on anhedonia—a loss of interest in previously enjoyed activities—as a consequence of continued stimulant use. Accordingly, for individuals with stimulant use disorder, drug use becomes the central means for obtaining enjoyment, and hence BA will augment HIV risk reduction counseling.
close
PrEP N’ Shine
Name of Grant
Developing and pilot testing an adaptive intervention to facilitate PrEP uptake and maximize PrEP adherence among at-risk transgender women.
Funding Source
National Institute of Mental Health (R34 MH122499-01A1)
Pls
Mimiaga and Biello
Background
PrEP has dramatically changed the promise of HIV prevention, particularly for transgender women (TGW) who are among the highest risk group for HIV in the U.S. While PrEP reduces HIV acquisition by >90% with adequate adherence, TGW face multiple transgender-specific barriers with PrEP access, uptake, adherence, and retention. The PIs have longstanding partnerships with community-based organizations that provide gender-affirming services to this group in Providence, RI and operate one of the first clinical PrEP programs in the U.S., led by our team at Miriam Hospital/Brown University.
Conceptual Model
The intervention package (“PrEP N’ Shine”) is based on over a decade of formative and programmatic work grounded in the social-cognitive and contextual realities of high-risk TGW, and as such, the conceptual model underlying the intervention draws on Empowerment Theory and Social Cognitive Theory. The “PrEP N’ Shine” package includes two separate but complementary interventions: 1) peer-led, strengths-based case management (SBCM) for PrEP linkage and uptake; and 2) a resource-efficient, adaptive “stepped-care” technology and counseling intervention to optimize PrEP adherence. “Stepped-care” is a healthcare delivery model in which the least resource intensive part of an intervention is delivered first, and only those who continue to have problems adhering to PrEP receive the more resource-intensive components.
Approach
Initially, we will continue to work with community members and a community advisory board to further inform the “PrEP N’ Shine” intervention (Aim 1a). Next, we will iteratively refine the intervention, in an open pilot trial with exit interviews, with up to 10 TGW to enhance participant acceptability, feasibility of study procedures, and finalize study protocols (Aim 1b). For Aim 2, we will conduct a pilot randomized controlled trial (RCT) of the “PrEP N’ Shine” intervention using a 2-stage randomization design: For Stage 1, we aim randomize 106 TGW who are candidates for PrEP to receive either the peer-led SBCM for PrEP linkage and uptake or standard of care (SOC; i.e., PrEP referrals only). For Stage 2, those from Stage 1 who initiate PrEP (n~44), regardless of their randomization condition, will then be equally re-randomized to either the resource-efficient, adaptive “stepped-care” intervention to optimize PrEP adherence (initially TGW in this arm will receive daily 2-way gender-affirming text message reminders, and then those continuing to have poor adherence will receive the 4 more intensive counseling sessions) or the SOC condition. Primary outcomes include PrEP linkage and uptake; PrEP adherence (both biomedical and self-report assessments); and retention in PrEP care.
Innovation
The “PrEP N’ Shine” intervention is highly scalable and sustainable in the real world, as it takes into account the “future of PrEP access,” while simultaneously 1) addressing the barriers surrounding access, 2) aiding in navigating linkage, and for those who need it, both insurance and free PrEP program options, and 3) reducing barriers to, and building skills to support, PrEP adherence (once TGW have access to PrEP).
close
Positive STEPS
Name of Grant
Adaptive intervention strategies trial for strengthening adherence to antiretroviral HIV treatment among youth
Funding Source
National Institute of Nursing Research (1R01NR017098-01)
Pls
Mimiaga and Garofalo
Background
A significant and growing population of young people are acquiring and living with HIV in the US. An estimated >12,200 adolescents were diagnosed with HIV infection in 2010, a 22% increase since 2008(1). Although HIV can be managed with ongoing antiretroviral therapy (ART), exceptionally high levels of adherence are required. Our recently published systematic literature review found that of the 21 articles published that reported data on medication adherence in HIV infected adolescents, seven described pilot interventions to enhance medication adherence; and only two utilized education / counseling sessions to promote adherence skills-building – a component that has shown to be necessary to improving adherence among HIV-infected adults. To our knowledge, there are no demonstrated efficacious ART adherence interventions for HIV infected adolescents to date. This is particularly concerning given that overall rates of adherence among adolescents is generally suboptimal.
Overview of Proposal
This proposal is culmination of 6 years of formative work with this population, including conducting two pilot randomized controlled trials (RCT). The current study is to test the efficacy of a stepped-care “adaptive” ART adherence intervention (“Positive STEPS”) for HIV infected adolescents, ages 16 to 24. Stepped care is a healthcare delivery model in which the least resource intensive part of an intervention is delivered first, and only those who do not improve then receive the high intensity, more resource intensive part of an intervention.
Conceptual Model
The conceptual model is based on our formative work that led to the development of a theoretically-driven intervention curriculum (“Positive STEPS”), grounded in the social and contextual realities of HIV infected adolescents. Our intervention begins with 2-way daily text messaging aimed at improving ART adherence. For many adolescents (over 1/3 from our pilot RCT), text messaging is not sufficient to overcome the barriers to ART adherence. These individuals will then also receive the more intensive component based on general principles of cognitive-behavioral therapy. Informational, problem solving, and cognitive-behavioral “steps” are addressed over 5, in-person, intervention-counseling sessions (incorporating digital video vignettes that are specific to the adherence challenges faced by adolescents).
Overview of Research Plan
192 HIV infected adolescents, aged 16 to 24, and prescribed ART will be recruited in two major U.S. cities with excellent access to and research experience with the population. Participants will be equally randomized to: (1) “Positive STEPS” – a stepped care, adherence intervention with integrated technology and counseling; or (2) Standard of Care comparison group. Participants will be followed for one-year post-randomization. The primary outcomes are improvements in measures of ART adherence (i.e., Wisepill, HIV viral load, and self-report); secondary outcomes include improvements in CD4 cell count, HIV symptoms, and quality of life.
close
MWCCS
Name of Grant
Los Angeles CRS for the MACS/WIHS combined cohort study
Funding Source
National Heart, Lung, and Blood Institute (U01 HL 146333)
Pls
Background
The Multicenter AIDS Cohort Study (MACS) / Women’s Interagency HIV Study (WIHS) Combined Cohort Study (MACS/WIHS-CSS) is a collaborative research effort that aims to understand and reduce the impact of chronic health conditions—including heart, lung, blood, and sleep (HLBS) disorders—that affect people living with HIV. For decades, the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health (NIH), has supported the separate MACS and WIHS cohort studies. MACS was a study of gay and bisexual men, while WIHS was a study of women who had other risk factors for HIV. The Multicenter AIDS Cohort Study is the first (1984) and largest study specifically created to examine the natural history of AIDS. This study involves 7,000+ gay and bisexual men nationwide; the UCLA site is the largest. The study has produced ~1500 papers and contributed landmark findings on the epidemiology of HIV infection and the virologic, immunologic, psychosocial, clinical and neurologic aspects of the disease. In 2019, the NHLBI became the primary steward of the new MACS/WIHS-CSS. The Combined Cohort Study includes continuing participants from the earlier studies. We are also recruiting new participants with a special focus on hard-hit population groups, such as Black/African American and Hispanic/Latinx men and women and residents of southern states.
close
Life Skills Mobile
Name of Grant
Digital, Limited Interaction Efficacy Trial of LifeSkills Mobile to Reduce HIV Incidence in Young Transgender Women
Funding Source
National Institute of Allergy and Infectious Diseases (1U01AI156875-01)
Pls
Mimiaga, Belzer, and Kuhns
Background
Young transgender women (YTW) have the highest HIV prevalence/incidence than any other risk group in the U.S. The repeated exposure to gender minority stigma compounded by the psychosocial challenges associated with social disadvantage and economic marginalization exacerbates disparities in HIV incidence and invalidates YTW’s gender identity. This can lead to behaviors (e.g., substance use, sex work, healthcare avoidance) that potentiate HIV acquisition risk. In order to decrease HIV incidence among YTW, an intervention needs to 1) address HIV risk as part of YTW’s life contexts; 2) be accessible and far-reaching such that the entire at-risk population can participate (e.g., rural areas) during a time most convenient for them; and 3) be highly sustainable with low associated costs to implement in real-world settings.
Conceptual Model
LifeSkills Mobile is an mHealth intervention to promote biobehavioral HIV prevention strategies based on empowerment theory and was developed using a community-based participatory research approach.
Overview of Study Design
We propose to conduct an RCT to assess the efficacy of the LifeSkills Mobile intervention in comparison to a standard of care (SOC) condition among 5,000 YTW recruited online. The primary outcome is reduction in incident HIV infections; a secondary outcome is total condomless anal/ vaginal sex acts occurring in the context of insufficient PrEP protection. At baseline and every 6 months through 48 months, enrolled participants will complete an online survey sent via a link to their mobile phone and will be mailed an OraQuick In-Home HIV Test kit . We will also estimate the total and incremental costs of the LifeSkills Mobile intervention relative to SOC, from healthcare sector and societal perspectives. Real World Applicability. Given inherent limitations to widespread dissemination of face-to-face, group-based interventions, LifeSkills Mobile extends the potential reach of the intervention via the development of a mobile version, and provides content on, and access to, current biobehavioral prevention technologies (e.g., PrEP).
close
Fostering Resilience Among MSM in India
Fostering Resilience to Psychosocial and HIV Risk in Indian MSM, 2014-2021
MPI: Safren & Mimiaga
National Institute of Mental Health (R01MH100627-01A1)
This was a randomized controlled efficacy trial of an HIV risk reduction group and individual counseling intervention that uses principles of cognitive behavioral therapy and emphasizes the importance of self-acceptance among MSM in Chennai and Mumbai, India.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper
Protocol Paper
Secondary Outcome Paper 1
Secondary Outcome Paper 2
Secondary Outcome Paper 3

PASSOS POSITIVOS
Name of Grant
Making universal, free-of-charge antiretroviral therapy work for sexual and gender minority youth in Brazil
Funding Source
National Institute of Mental Health (R34 MH126894-01)
Pls
Matthew Mimiaga and Katie Biello
Background
Sexual and gender minority (SGM) youth account for the largest number of incident HIV infections in Brazil. Although HIV can be managed with ongoing antiretroviral therapy (ART), exceptionally high levels of adherence are required. Brazil has implemented a comprehensive HIV treatment program with broad access to ART, but this program does not specifically address barriers to optimal ART adherence, particularly for SGM youth who experience many challenges taking their medication as prescribed.
Overview
This application seeks to develop and pilot test a theory-based, integrated technology and counseling intervention to improve ART adherence among HIV infected SGM youth (ages 15-24) in Rio de Janeiro, Brazil. The intervention aims to improve social support, self-efficacy for taking ART, and teach skills for problem-solving barriers to promote better adherence. To inform the content, structure, and format of the proposed intervention, the MPIs recently conducted focus groups with SGM youth (N = 18) and key informant interviews (N = 7) with medical providers and staff at local HIV service organizations working closely with SGM youth in Rio de Janeiro. Across focus groups and key informant interviews there was universal agreement that an intervention should capitalize on and enhance social support structures among SGM youth, and address their specific concerns, especially as related to the individual (e.g., ART side effects, mood, substance use), social (e.g., HIV/SGM stigma), and structural (e.g., clinic hours, transportation challenges) barriers that they regularly face.
Theoretical Model
The intervention is guided by Social Cognitive and Social Support Theories and is grounded in the social and contextual realities of SGM youth living with HIV in Brazil. Specifically, social support is emphasized and informational, problem-solving and cognitive-behavioral “steps” are addressed over 4-group adherence counseling sessions, which include short video vignettes that seek to normalize adherence challenges. In addition, daily tailored SMS text messages are delivered as part of the intervention to facilitate social-cognitive cues to take medications as prescribed.
Research Plan
Phase 1: Refine and enhance participant acceptability of the intervention and resolve any issues with intervention delivery/implementation; this will be achieved by convening and obtaining feedback from our youth community advisory board throughout this phase and subsequent phases; and by conducting an open-phase pilot with up to 12 SGM youth, with post-intervention exit interviews, as well as obtaining feedback from our youth community advisory board throughout this and subsequent phases. Phase 2: Examine, in a pilot randomized controlled trial, the feasibility, acceptability and potential impact of the proposed intervention among 72 SGM youth who will be equally randomized to the intervention or a time- and attention-matched control condition with standard of care. The outcomes are improved ART adherence (Wisepill, pharmacy assessment and self-report), retention in care and viral load suppression. Study assessments will be conducted at baseline, 3- and 6-months.sss
close
Project LifeSkills
-
- HIV Prevention Intervention for Young Transgender Women, 2011-2016
MPI: Garofalo & Mimiaga; Co-Is: Kuhns & Reisner
National Institute of Mental Health (R01MH094323-01)
Randomized clinical efficacy trial of Project LifeSkills, a group-delivered, behavioral HIV prevention intervention, vs standard of care conducted among 190 sexually active YTW between March 26, 2012, and August 15, 2016, at community-based locations in Boston, Massachusetts, and Chicago, Illinois, to reduce sexual risk for HIV acquisition or transmission.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper
Protocol Paper
Administrative Supplement Paper
Secondary Outcome Paper 1
Secondary Outcome Paper 2
Secondary Outcome Paper 3
Secondary Outcome Paper 4
Secondary Outcome Paper 5
Secondary Outcome Paper 6
Secondary Outcome Paper 7
Secondary Outcome Paper 8
Secondary Outcome Paper 9
Secondary Outcome Paper 10
Secondary Outcome Paper 11
Secondary Outcome Paper 12
Secondary Outcome Paper 13
Secondary Outcome Paper 14
- HIV Prevention Intervention for Young Transgender Women, 2011-2016
- Mobile Adaptation and Testing of a Uniquely Targeted HIV Intervention for Young Transgender Women, 2019-2020
MPIs: Kuhns & Mimiaga
National Institute of Mental Health (R56MH113684-01)
The group-based LifeSkills intervention was adapted to a mobile app, LifeSkills Mobile, with input from an expert advisory group and feedback from YTW collected during user-centered design sessions. A beta version of the app was then tested in a usability evaluation using a think-aloud protocol with debriefing interviews, recordings of screen activity, and assessments of usability
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper
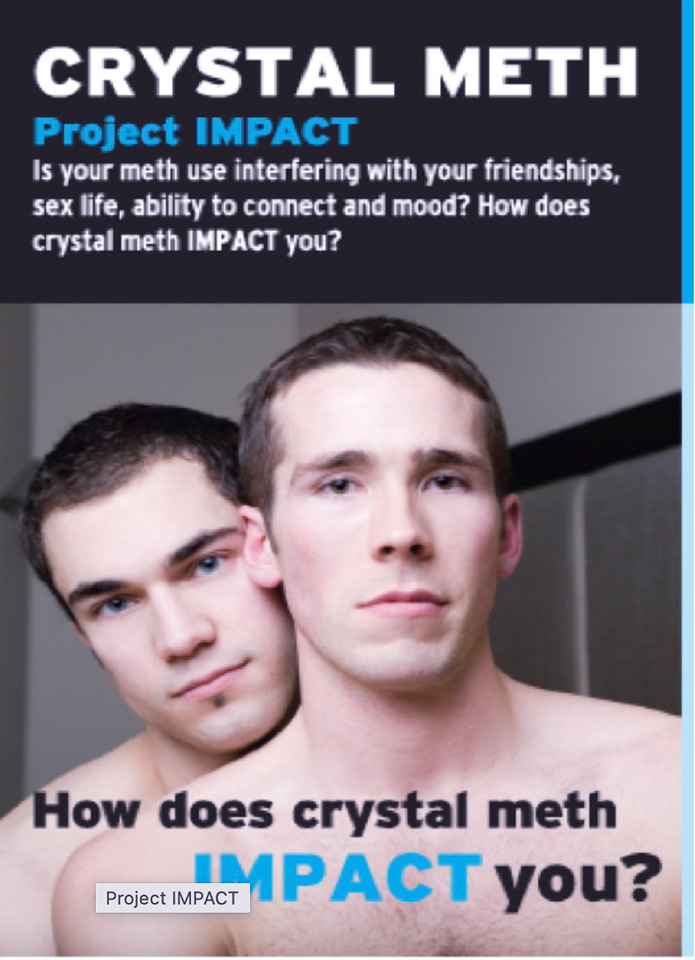
Project IMPACT
-
- Behavioral Activation and HIV Risk Reduction for MSM with Crystal Meth Abuse, 2011-2015
PI: Mimiaga
National Institute on Drug Abuse (R34DA031028-01)
Findings provide further evidence of feasibility and acceptability, and demonstrate initial efficacy for reducing sexual risk for HIV and crystal methamphetamine use in a pilot RCT.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper
Protocol Paper
- Behavioral Activation and HIV Risk Reduction for MSM with Crystal Meth Abuse, 2011-2015
- Behavioral Activation and HIV Risk Reduction for MSM with Crystal Meth Abuse, 2008-2010
PI: Mimiaga
National Institute on Drug Abuse (R03DA023393-01)
Findings provide evidence of feasibility and acceptability, and demonstrate initial efficacy for reducing sexual risk for HIV and crystal methamphetamine use in an open pilot trial.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper
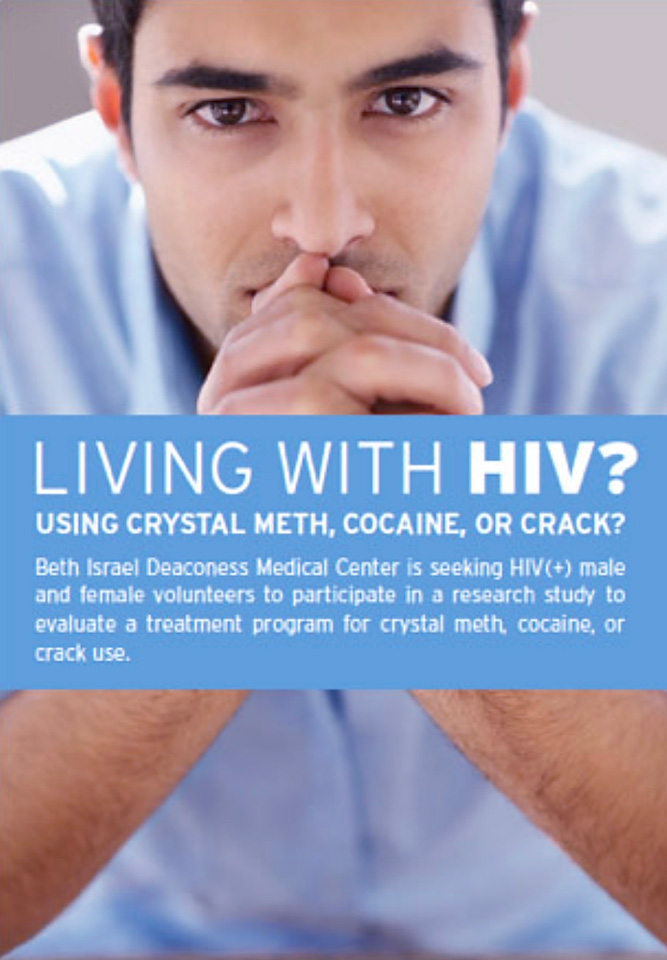
Project REWARD
Sustaining Effects of Contingency Management on Stimulant Use In HIV-Infected Persons, 2011-2014
MPI: Mimiaga & Mitty
Harvard Center for AIDS Research Award
We developed and implemented a combined contingency management (CM) and behavioral activation intervention aimed at HIV-infected individuals who are engaged in HIV care and currently dependent on crack, cocaine, or methamphetamine. Findings provide evidence of feasibility and acceptability, and demonstrate initial efficacy for improvements in ARV medication adherence.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
close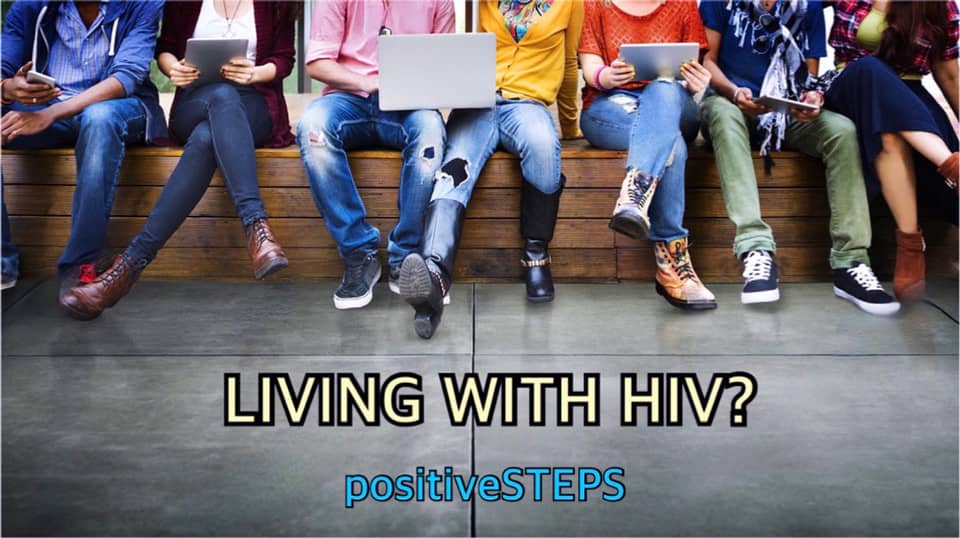
Positive STEPS
Improving Antiretroviral Medication Adherence Among HIV-Infected Youth, 2011-2013
PI: Mimiaga
Harvard Center for AIDS Research Award
This study adapted the Life-Steps intervention designed by our group for HIV-infected adults to be responsive to the needs of HIV-infected adolescents. Following an intervention development phase involving qualitative interviews with 30 adolescents, we conducted an RCT pilot of the intervention among 30 HIV-infected adolescents.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper 1
Primary Outcome Paper 2
Secondary Outcome Paper
Protocol Paper
Description of the Intervention Paper

Stronger Together
CVCTPlus: A Couples-Based Approach to Linkage to Care and ARV Adherence, 2013-2018
MPI: Mimiaga, Stephenson & Garofalo
National Institute of Child Health and Human Development (R01HD075655-01A1)
We conducted a randomized controlled efficacy trial of a behavioral intervention that included CVCT combined with dyadic adherence counseling (“CVCTPlus”) to improve linkage to care, retention in care, ART adherence and viral suppression among 250 (total N = 500) HIV serodiscordant male-male couples across Atlanta, Boston, and Chicago. Findings demonstrated efficacy for improving HIV care continuum outcomes.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper
Protocol Paper
Description of the Intervention Paper
Secondary Outcome Paper 1
Secondary Outcome Paper 2
Secondary Outcome Paper 3
Secondary Outcome Paper 4
Secondary Outcome Paper 5
Secondary Outcome Paper 6
Secondary Outcome Paper 7
Secondary Outcome Paper 8
Secondary Outcome Paper 9
Secondary Outcome Paper 10
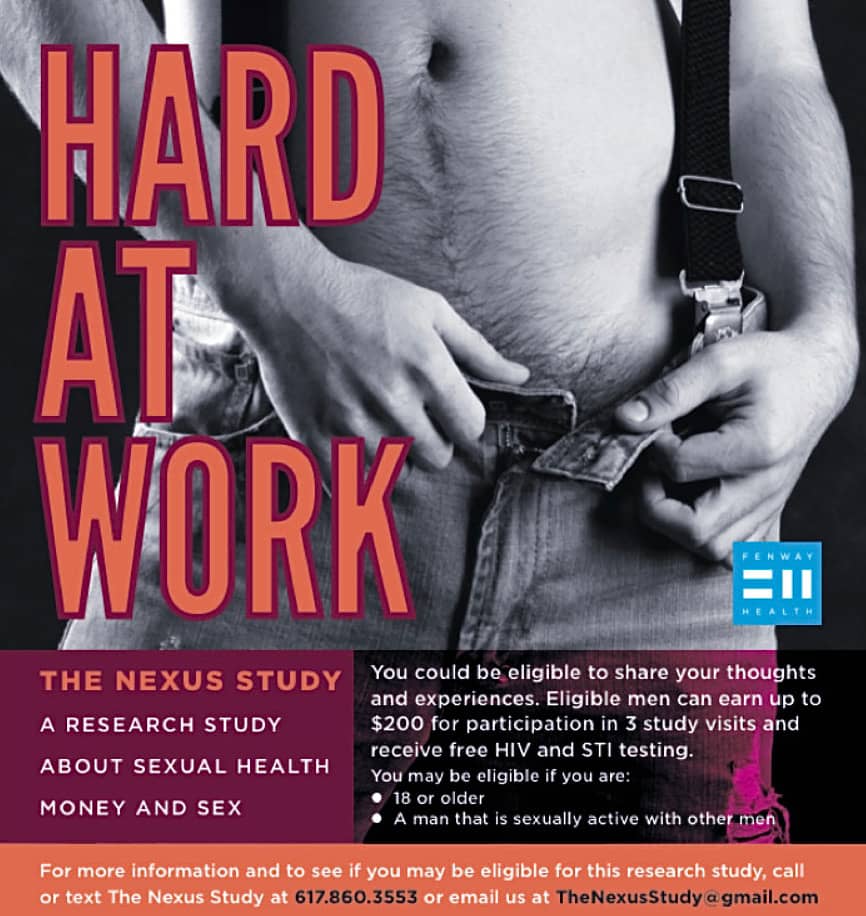
NEXUS Study
-
- HIV Risk for MSM Sex Workers: A Social, Sexual and Drug Network Simulation Study, 2013-2016
MPI: Mimiaga & Biello
National Institute on Drug Abuse (R21DA035113-01A1)
This was a longitudinal epidemiological study of MSM sex worker networks in Massachusetts and Rhode Island to identify protective and risk factors that affect HIV transmission dynamics. Longitudinal data enhanced our understanding of how contemporary social, sexual, and drug abuse network characteristics contribute to increased HIV and STI spread among male sex workers.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper 1
Primary Outcome Paper 2
Primary Outcome Paper 3
Secondary Outcome Paper 1
Secondary Outcome Paper 2
Secondary Outcome Paper 3
Secondary Outcome Paper 4
Secondary Outcome Paper 5
- HIV Risk for MSM Sex Workers: A Social, Sexual and Drug Network Simulation Study, 2013-2016
- HIV Risk Among Male Sex Workers in New England
PI: Mimiaga
The Fenway Institute, Fenway Health Seed Award
This was a formative study to lay the groundwork for a larger network-based study of male sex workers.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper 1

Inkwari: Umlazi, Durban, SA
Inkwari: An Emerging High-Risk Place Potentiating HIV Spread Among Young Adults in a Hyper-Endemic South African Setting, 2011-2014
PI: Mimiaga
Ragon Institute of MGH, MIT and Harvard Scholars Award
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper
Secondary Outcome Paper 1
Secondary Outcome Paper 1

Whoonga: Recreational ARVs South Africa
Epidemiology of HIV Antiretroviral Exposure from Whoonga Use in South Africa, 2015-2018
MPI: Grelotti & Mimiaga
National Institute on Drug Abuse (R21DA039857-01)
Some people are exposed to HIV antiretroviral medication through recreational use. This emerging phenomenon poses a significant obstacle to efforts to address the global HIV pandemic. Any antiretroviral exposure from recreational use may increase rates of antiretroviral-resistant HIV strains. This and any diversion of antiretroviral medication for recreational use will increase the cost of delivering this life-saving care. The proposed research will document antiretroviral exposure from the use of whoonga, a drug cocktail in South Africa that may contain antiretroviral medication and illicit drugs. It will also inform future research to link recreational antiretroviral use to antiretroviral resistance among HIV-infected individuals who have yet to initiate HIV treatment, as well as promote the design of culturally appropriate interventions.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper
Formative Paper 1
Formative Paper 2
News Related Article

Men’s Small Group Vietnam
- Sexual Health Needs of Male Sex Workers in Ho Chi Minh City, Vietnam, 2010-2012 MPI: Colby & Mimiaga
Harvard Catalyst Pilot Grant (UL1RR025758-01)The aim of this study was to conduct formative research to better understand risk and protective factors for HIV/STI transmission among MSW in Ho Chi Minh City.
-
Group Based HIV Prevention Intervention for MSW In Ho Chi Minh City, Vietnam 2013-2016
MPI: Mimiaga & Colby
Centers for Disease Control and Prevention – Vietnam
This was a pilot trial of a group-based manualized HIV prevention intervention, focused on barriers to HIV risk reduction and problem solving/skills building. The intervention consisted of 4 group sessions facilitated by trained MSM peer health educators.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper
Formative Paper 1
Formative Paper 2
Formative Paper 3
Formative Paper 4
Formative Paper 5
Formative Paper 6
Formative Paper 7
Testing Brief Messages
Testing Brief Messages for Black & Latino MSM: Emerging HIV Prevention Options, 2012-2015
PI: Mimiaga
Centers for Disease Control and Prevention / National Center for HIV, Viral Hepatitis, STDs, and TB Prevention (U01PS0053307-01)
This study included Black and Latino MSM in three major US cities—Chicago, Fort Lauderdale, and Kansas City— with variation in HIV serostatus and sexual risk behavior. Brief health messages of biomedical (e.g., PrEP, PEP, ARVs for treatment) and behavioral (e.g., condoms, serosorting) HIV prevention options were created through extensive qualitative interviews, key informant interviews, and focus groups with these populations. These data were used to refine the messages per participant and expert feedback, and to ensure comprehension of information / health literacy, clarity, increase in knowledge, and potential to influence behaviors and attitudes. Through an iterative approach, the messages were further refined and finalized. The final phase tested the brief messages (delivered via text message) on health behavior change among 1500 Black and Latino MSM in the same three cities. The primary aim of this project was to assess changes in behaviors and attitudes, feasibility of message delivery, and acceptability of message content.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper
Secondary Outcome Paper 1
Secondary Outcome Paper 2
Secondary Outcome Paper 3
Secondary Outcome Paper 4
Secondary Outcome Paper 5
Secondary Outcome Paper 6
Secondary Outcome Paper 7

Club Drugs & PrEP
Understanding PrEP Implementation Among Club Drug Using MSM, 2011-2014
MPI: Mimiaga & Mitty
National Institute of Mental Health (R21MH095535-01)
This study reports finding on PrEP implementation approached among club drug using MSM.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper 1
Primary Outcome Paper 2
Primary Outcome Paper 3

mHealth Male Sex Workers India
Technology For HIV Prevention Among Vulnerable Men in India, 2011-2015
PI: Mimiaga
National Institute on Drug Abuse (R21DA03372-01)
We first conducted qualitative interviews and focus groups to inform the content, structure and format of an HIV risk reduction intervention for male sex workers in India. We then conducted an open pilot of the intervention and assessed initial feasibility and acceptability. Next, we conducted a pilot randomized controlled trial of a mobile phone delivered HIV prevention intervention among this group.
PUBLISHED SCIENTIFIC JOURNAL ARTICLES:
Primary Outcome Paper 1
Primary Outcome Paper 2
Secondary Outcome Paper

PrEPare for Work
Name of Grant
Efficacy of a PrEP uptake & Adherence Intervention among male sex workers using a 2-stage randomization design
Funding Source
National Institute of Nursing Research (R01NR020227-01A1)
Pls
Katie Biello, Matthew Mimiaga, and Philip Chan
Background:
Male sex workers (MSWs), or men who exchange sex for money, goods, drugs, or other items of value with other men, are at exceptionally high risk for HIV infection. Pre-exposure prophylaxis (PrEP) is effective at reducing HIV acquisition among HIV uninfected individuals, but its efficacy is highly dependent on uptake and excellent adherence. However, uptake of and adherence to PrEP among those who might benefit the most from using PrEP, such as MSWs, remains suboptimal. A successful PrEP uptake and adherence package must be responsive and tailored to MSWs’ distinct psychosocial and contextual circumstances.
Overview of Proposal
The current proposal is a culmination of over 10 years of research with this population, including qualitative research, epidemiological assessments and programmatic work. These formative data led to an NIMH-funded R34 (MPIs: Biello, Mimiaga, Chan), which allowed our interdisciplinary team and community partners to collaborate on the development and pilot testing of a theory-based intervention— “PrEPare for Work”—to address 1) access to and uptake of PrEP at local PrEP clinics/providers via strengthbased case management using principles of motivational interviewing (e.g., focusing on values, strengths and change efforts, making reflective and empathetic statements), and 2) provide cognitive-behavioral therapyinformed PrEP adherence counseling (e.g., problem-solving skill-building) with personalized, daily text message reminders to optimize PrEP adherence among MSWs. The pilot RCT demonstrated the feasibility, acceptability and preliminary efficacy of “PrEPare for Work”.
Conceptual Model
The “PrEPare for Work” intervention is based on Social Cognitive Therapy (SCT), which specifies a core set of mechanisms that influence health behavior with a primary emphasis on self-regulation and self-reflection, including self-efficacy.
Overview of Study Design
We now propose to test the efficacy of the “PrEPare for Work” package in the Greater Providence area and in Los Angeles County using a two-stage randomization design. Stage 1: 500 MSW will be equally randomized to receive either the “PrEPare for Work Stage 1 intervention” (strength-based case management and facilitated PrEP linkage) or standard of care to evaluate successful PrEP uptake (verified by real-time tenofovir urinalysis; prescription data) within 2 months. Stage 2: those who initiate PrEP (n~156; ~55% from Stage 1 intervention arm and ~20% from Stage 1 SOC arm) will be equally re-randomized to the “PrEPare for Work Stage 2 intervention” (1-on-1 skills training, problem solving, and motivational interviewing adherence counseling and personalized, daily text messaging reminders) or SOC to assess PrEP adherence (tenofovir concentration in hair sample) and retention in PrEP care (appointments attended) over 12 months. We will also examine the degree to which improvements in PrEP uptake and adherence occur in the context of the conceptual mediators (e.g., PrEP motivation, self-efficacy) and moderators (e.g., race/ethnicity, substance use, perceived HIV risk) of the intervention. Intervention cost-effectiveness will be assessed.
close
Fostering Resilience
Name of Grant
Fostering resilience to psychosocial and HIV risk in Indian MSM
Funding Source
National Institute of Mental Health (R01MH100627-01A1)
Pls
Mimiaga and Safren
Background
India has the world’s third largest HIV epidemic1, and given the population size, one of the largest, if not the largest, populations of men who have sex with men (MSM) in the world. MSM in India have an estimated seroprevalence of 14.7%. HIV prevention efforts for MSM in India are limited to condom distribution and HIV education, with no existing efficacy trials of interventions and therefore no evidenced based interventions this population. They are hidden, stigmatized, and face considerable psychosocial stressors, including pressure to marry, which increases the risk for HIV transmission to their wives. This proposal is the culmination of our ongoing, successful > 10-year community-based research collaboration with two NGOs dedicated to HIV prevention among MSM, Sahodaran (Chennai) and The Humsafar Trust (Mumbai), and investigators from the India Council of Medical Research (ICMR), National Institute for Research in Tuberculosis (NIRT) in Chennai. We have, in every phase of the development of this proposal (and throughout each of our preliminary studies), engaged the community in developing the research ideas, forming the program of research, designing / refining the studies, and disseminating the results to inform next-steps. Preliminary studies include: 1) documenting the exceptionally high rates of distress / mental health problems in MSM in Mumbai, 2) documenting, in Chennai, the high prevalence of HIV and sexual risk, and the important surrounding psychosocial context, 3) conducting a three-phased Indo-U.S. sponsored R21 including extensive formative work from CABs, focus groups with representative MSM, and key informant interviews to develop our self-acceptance based model of self-care in the context of pervasive stigma and discrimination facing Indian MSM. We field tested and then conducted a feasibility pilot RCT (with CAB feedback throughout) of the resulting intervention comparing it to HIV voluntary counseling and testing (VCT) alone. This field test and pilot RCT showed high participant acceptability and feasibility of study procedures, and success reducing HIV sexual risk behavior.
Design
MSM in Chennai and Mumbai will be randomized to either: 1) a self-acceptance based HIV sexual risk reduction intervention and HIV/STI VCT, or 2) HIV/STI VCT. Those randomized to the experimental intervention will receive 4 group sessions focused on building self-acceptance, social support and HIV risk reduction skills and 6 individual sessions focused on personalized HIV risk reduction plans and, as needed, prevention case management. Participants will be followed for one year, with STI incidence and HIV risk behavior as primary outcomes and psychosocial mediators secondary. Cost effectiveness of the intervention will be calculated compared to HIV/STI VCT alone, considering individual and public health benefits as well as downstream cost-savings due to infections averted.
close
IMPACT – ATN 170
Name of Grant
Hybrid Type 2 Effectiveness-Implementation Trial of Status Neutral, Integrated Behavioral Activation and Risk Reduction Intervention for Stimulant Use Among Sexually Active Young GBMSM
Funding Source
National Institute of Child Health and Human Development / Adolescent Medicine Trials Network for HIV Interventions (ATN170)
Pls
Mimiaga and Biello
Background
Stimulant (e.g., crystal methamphetamine, cocaine, ecstasy, MDMA) use is a substantial public health problem among young gay, bisexual and other men who have sex with men (YGBMSM) in the United States (US); the prevalence of past-year use is 2x greater among YGBMSM compared to their heterosexual counterparts. Use of stimulants may lead to behavioral disinhibition and facilitate, prolong, and enhance sexual activity, contributing to increased engagement in sexual risk behaviors, including condomless anal sex (CAS), and HIV & STI acquisition and transmission. In the US, as high as 33% of YGBMSM report having ever used stimulants in the context of sex. Stimulant use often co-occurs with other psychosocial problems (e.g., depression), further increasing HIV vulnerability among YGBMSM. Stimulant use also hinders the use of prevention services, such as uptake/adherence to pre-exposure prophylaxis (PrEP). Similarly, for YGBMSM living with HIV, stimulant use leads to suboptimal antiretroviral therapy (ART) adherence, poor retention in HIV care and unsuppressed viral load, which impedes treatment-as-prevention (TasP) efforts and leads to devastating HIV-related health outcomes
Design
This is a Hybrid Type 2 Effectiveness-Implementation Trial. The reach and effectiveness of Project IMPACT will be tested in a two-arm, multi-site and multi-format (i.e., in-person and virtual) randomized controlled trial of 360 cisgender YGBMSM who use stimulants in the context of high-risk sex. Project IMPACT, a status neutral, psychosocial intervention that uses behavioral activation (BA)—an evidence-based, cognitive behavior therapy—as a treatment for stimulant use and sexual risk reduction counseling for GBMSM. The experimental condition (BA-RR) is comprised of 10 sessions—one session focused on orienting and rationale, two sessions focused on risk reduction, six sessions integrating BA and risk reduction counseling (including PrEP or ART and HIV care), and one final session on relapse prevention.

close
Scientific Publications
STAY INFORMED
AND INSPIRED









AVAILABLE POSITIONS
Open Positions: 1) Biostatistician, 2) Research Associate, 3) Medical Director, 4) Two Administrative Assistants, and 5) Retention Specialist
Open Positions!

UCLA Fielding School of Public Health Establishes Center to Focus on the Health, Safety and Well-being of LGBTQ Community

The Persistent and Evolving HIV Epidemic in American Men Who Have Sex With Men

Group led by UCLA professor awarded $8.8 million for HIV intervention using mobile app

Strengthening Resilience to Reduce HIV Risk in Indian MSM: a Multicity, Randomised, Clinical Efficacy Trial
What We’ve Learned About Disease in the 40 Years Since the Discovery of HIV/AIDS at UCLA
Promoting Public Health for the LGBTQ Population
A new FSPH center will partner with community groups and policymakers to develop and implement evidence-based strategies that advance the physical and mental health of sexual and gender minorities.

Dr. Matthew Mimiaga, a professor of epidemiology widely known for his work with sexual and gender minorities, heads the new FSPH center.
“As a member of the LGBTQ community, I know what it’s like to experience discrimination and fear around my sexual identity. I look forward to the impact C-LARAH will have in training future generations of scientists interested in conducting LGBTQ public health research.” — Dr. Matthew Mimiaga

Fielding School Professor’s Team Awarded more than $5.2 Million in Grants for HIV Prevention
A team of researchers co-led by UCLA Fielding School of Public Health epidemiology professor Dr. Matthew Mimiaga has received more than $5.2 million in grants from the U.S. National Institutes of Health (NIH) to develop and test interventions in the U.S. and Brazil. The projects, funded by three separate NIH grants, all have the goal of reducing the spread of HIV, the virus that causes AIDS, through the use of antiretroviral medications for HIV primary (PrEP) and secondary (ART) prevention among sexual and gender minority groups. “Whether used as PrEP for HIV negative individuals or as ART treatment as prevention for those living with HIV, antiretroviral medications are highly effective at reducing HIV acquisition and transmission, but its efficacy is highly dependent on uptake and excellent adherence,” said Mimiaga, director of the UCLA Center for LGBTQ Advocacy, Research & Health. “However, sexual and gender minority groups face specific barriers to PrEP and ART access, uptake, adherence, and retention in care. Because of this, we are testing interventions that are culturally-tailored to address the lived realities and barriers among these vulnerable groups.” The grants, announced by the NIH this month, will study the use of a variety of techniques – personalized, daily text message reminders; video vignettes; peer navigation; and individual and group counseling – to facilitate access and adherence to antiretroviral medications among those who would benefit the most from its use. These grants will be implemented in Los Angeles County; Providence, RI; Boston, MA; and Rio de Janeiro, Brazil. This will give the researchers a wide variety of data on how these approaches work for different populations, ranging from LGBTQ adolescents, ages 15-24, to transgender women, and men who engage in transactional sex with other men. Dr. Katie Biello, a Brown University behavioral and social sciences and epidemiology professor, will co-lead this work with Mimiaga. “Our goal is to develop HIV prevention interventions that are highly scalable and sustainable in the real world,” Biello said. “As such, this work takes into account the future of PrEP and ART access, while simultaneously addressing the barriers surrounding access, aiding in navigating linkage to PrEP and ART care programs, and reducing barriers to, and building skills to support, medication adherence.”
The UCLA Fielding School of Public Health, founded in 1961, is dedicated to enhancing the public's health by conducting innovative research, training future leaders and health professionals from diverse backgrounds, translating research into policy and practice, and serving our local communities and the communities of the nation and the world. The school has 631 students from 26 nations engaged in carrying out the vision of building healthy futures in greater Los Angeles, California, the nation and the world.
UCLA Fielding School Professor’s Team Awarded more than $5.2 Million in Grants for HIV Prevention
UCLA Fielding School Center for LGBTQ+ Advocacy, Research & Health Marks Its First Year
-
- Published 38 new scientific journal publications and five book chapters, which can be reviewed here. The findings were published in journals that include The Lancet, The Lancet Global Health, Drug and Alcohol Dependence, AIDS and Behavior, Journal of the International AIDS Society, Journal of AIDS, and AIDS;
- Collaborated with 37 UCLA graduate students, affiliated post-doctoral researchers, and staff, along with 20 faculty affiliates;
- Received nearly $8.6 million in federal research funding from five different U.S. National Institutes of Health entities in FY 2021 (>$50 million for all project years for current grants combined); and
- Built a website for the new center that spotlights C-LARAH’s research program.